Introduction to Urological Health and Fertility
Urological health is a critical aspect of overall well-being for American males, particularly when it comes to fertility. The field of urology encompasses a broad range of conditions that can affect the male reproductive system, including the kidneys, bladder, ureters, urethra, and the male reproductive organs. Understanding these conditions and their potential impact on fertility is essential for men who are planning to start a family or are experiencing difficulties in conceiving.
Common Urological Conditions Affecting Fertility
Several urological conditions can directly influence a man's fertility. Varicoceles, for example, are enlarged veins within the scrotum that can lead to reduced sperm quality. Studies have shown that varicoceles are present in about 15% of the general male population and up to 40% of men with primary infertility. Another condition, epididymitis, which is an inflammation of the epididymis, can also impair fertility by obstructing the passage of sperm.
Chronic prostatitis, an inflammation of the prostate gland, can cause pelvic pain and urinary symptoms, and may also affect sperm quality and function. Additionally, sexually transmitted infections (STIs) such as chlamydia and gonorrhea can lead to epididymitis or urethritis, further complicating fertility issues.
Diagnostic Approaches to Urological Fertility Issues
Diagnosing urological conditions that impact fertility typically involves a combination of medical history review, physical examination, and specialized tests. Semen analysis is a fundamental diagnostic tool that assesses sperm count, motility, and morphology. In cases where abnormalities are detected, further investigations such as scrotal ultrasound or transrectal ultrasound may be necessary to identify underlying issues like varicoceles or prostate abnormalities.
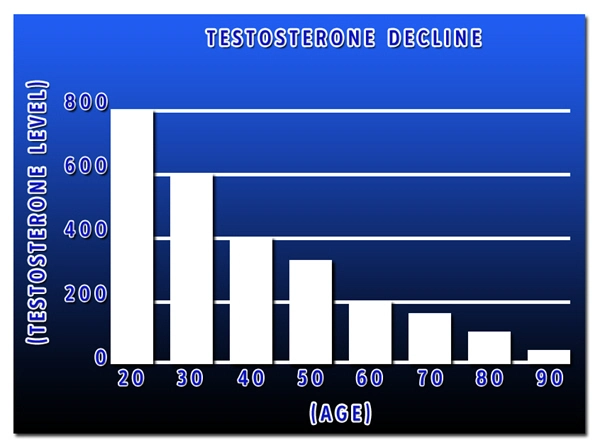
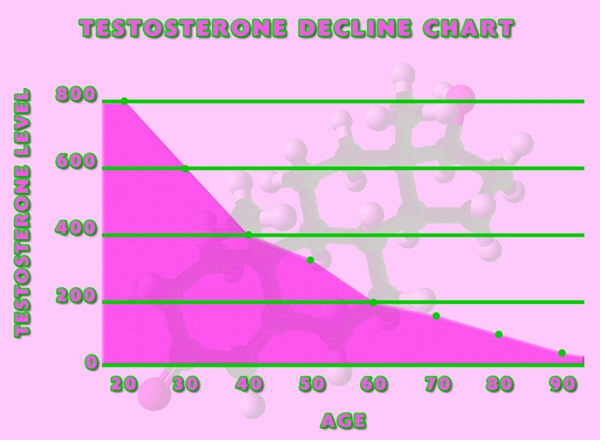
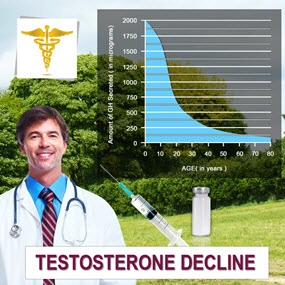
Hormonal assessments can also be crucial, as imbalances in hormones such as testosterone and follicle-stimulating hormone (FSH) can affect sperm production. Advanced diagnostic techniques, including genetic testing and post-ejaculatory urinalysis, may be employed in complex cases to pinpoint the cause of infertility.
Treatment Options and Fertility Restoration
The treatment of urological conditions affecting fertility varies depending on the specific diagnosis. For varicoceles, surgical intervention such as varicocelectomy can improve sperm parameters and increase the chances of natural conception. In cases of epididymitis or prostatitis, antibiotics and anti-inflammatory medications are often prescribed to manage infection and inflammation.
For men with obstructive azoospermia, where sperm production is normal but blocked, surgical procedures like vasoepididymostomy or vasovasostomy can restore the passage of sperm. In situations where fertility cannot be restored through surgery, assisted reproductive technologies (ART) such as in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI) offer viable alternatives.
Preventive Measures and Lifestyle Considerations
Preventive measures play a significant role in maintaining urological health and optimizing fertility. Regular check-ups with a urologist can help detect issues early and manage them effectively. Lifestyle factors such as maintaining a healthy weight, avoiding tobacco and excessive alcohol, and protecting the genital area from excessive heat can also contribute to better fertility outcomes.
Moreover, practicing safe sex to prevent STIs and maintaining good hygiene are essential steps in preserving urological health. For men with a family history of urological conditions, genetic counseling may provide additional insights and preventive strategies.
Conclusion: Empowering American Males Through Knowledge and Action
In conclusion, understanding the relationship between urological conditions and fertility is vital for American males. By being informed about common conditions, diagnostic approaches, treatment options, and preventive measures, men can take proactive steps to safeguard their reproductive health. Collaboration with healthcare providers, particularly urologists and fertility specialists, is key to addressing fertility challenges and achieving the goal of starting or expanding a family.
Contact Us Today For A Free Consultation

- Urological Health Guide: Proactive Care and Common Conditions for American Men [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Urological Health Guide for American Men: Symptoms, Conditions, and Preventive Care [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Smoking's Detrimental Effects on Urological Health in American Men: A Comprehensive Overview [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Genetics and Urological Health in American Men: Prostate Cancer, BPH, Kidney Stones, Infertility [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Cardiovascular and Urological Health: A Vital Connection for American Men's Wellness [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Urological Infections in American Males: Causes, Prevention, and When to Seek Help [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Trends and Innovations in Urological Care for American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Managing Urological Pain in Men: Causes, Diagnosis, and Treatment Options [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Veterans' Urological Care: Specialized Services and Holistic Health Support [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Urological Health Strategies for American Men in the Workplace [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Exercise Regimen for American Men to Boost Urological Health [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hydration's Role in Enhancing Urological Health for American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Urological Health in Sports: Risks, Prevention, and Performance for American Male Athletes [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Urological Rehabilitation: Enhancing Men's Health and Quality of Life in America [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Urological Health's Psychological Impact on American Males: Breaking the Silence [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Stress Impact on Urological Health in American Males: Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Debunking Urological Myths: Essential Facts for American Men's Health [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Technological Advances Revolutionizing Urological Diagnosis for American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Urological Health and Mental Well-being: A Holistic Approach for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Navigating Urological Insurance: A Comprehensive Guide for American Men's Health [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Urological Health in American Men: Screenings, Conditions, and Holistic Care [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Health Education: Vital for American Males' Quality of Life [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Health Guide for American Males: Best Practices and Preventive Care [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Health: Enhancing American Men's Quality of Life Through Proactive Care [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urological Health and Cancer: Prevention, Detection, and Treatment for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health: Key to Longevity for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Urological Health in American Men with Chronic Illnesses: A Comprehensive Guide [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Supplements for Urological Health: Benefits for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Alcohol's Impact on Urological Health: Risks and Management Strategies for Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health: Vital Screening and Care for Young American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Urological Health in Men Over 50: Strategies and Insights [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health and Skin Care: A Holistic Approach for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Urological Health and Mental Well-being: A Holistic Approach for Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Obesity's Impact on Urological Health in American Men: Risks and Management Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Environmental Impacts on Urological Health in American Males: Risks and Prevention [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health and Immunity: Strategies for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Surgery Recovery Guide for U.S. Males: Tips and Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health Guide for American Males: Procedures, Conditions, and Recovery [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Exercise and Urological Health: Safe Practices for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health and Medications: Effects, Management, and Screening for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health and Sleep: A Vital Connection for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health: Vital for American Men's Wellness and Quality of Life [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Dietary Guide for Enhancing Urological Health in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Urological Health's Impact on Sexual Function in American Men: Education and Awareness [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Urological Health and Fertility: A Guide for American Males Planning Families [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Urological Health: Essential Travel Tips for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Urological and Bone Health: Essential Connections for American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Urological Health's Impact on American Men's Social and Professional Lives [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Integrating Urological Health into U.S. Men's Health Campaigns: A Vital Step Forward [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Urological Health and Vision: A Critical Link for American Men's Wellness [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Urological Health and Hearing Loss: Connections and Risks in American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Urological Health in American Men: Research, Challenges, and the Need for Action [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Urological Health: A Vital Focus in U.S. Men's Health Advocacy [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Urological Health Linked to Dental Care: Insights for American Men's Well-being [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Urological and Respiratory Health Nexus: Critical Insights for American Males [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Urological Health: A Critical Focus for U.S. Men's Health Policy Enhancement [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Urological and Digestive Health: A Vital Connection for American Males [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Urological Health Education: Vital for American Men's Well-being and Quality of Life [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Urological Health's Impact on Men's Career Performance and Well-being [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Urological and Musculoskeletal Health Link: Insights for American Men's Wellness [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Urological Health's Impact on American Men and Family Life: A Holistic Approach [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Urological and Endocrine Health: A Vital Connection for Men's Wellness [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Urological Health Integration Enhances Men's Health Programs in America [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Neurological Impacts on Urological Health in American Males: Insights and Management [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Urological and Cardiovascular Health Links: Guidance for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Urological Health: Vital for Men's Well-being and Longevity [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Urological Health's Crucial Role in Men's Reproductive Well-being [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
Word Count: 573