Introduction
Hypogonadism, a condition characterized by low levels of testosterone, can significantly affect various bodily functions, including muscle activity. Recent studies have begun to explore the relationship between hypogonadism and pelvic floor electromyographic (EMG) activity, an essential aspect of male health that influences urinary and sexual function. This article delves into the modifications observed in pelvic floor EMG activity following targeted hormone replacement therapy (HRT) in hypogonadal men, providing valuable insights for American males dealing with this condition.
Understanding Hypogonadism and Its Effects
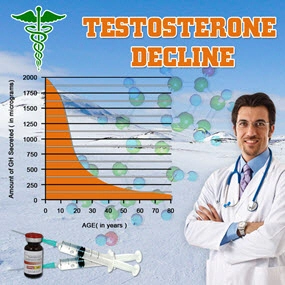
Hypogonadism in men results from the testes' inability to produce sufficient testosterone, leading to a myriad of symptoms such as decreased libido, fatigue, and muscle weakness. The pelvic floor muscles, crucial for maintaining continence and sexual function, are particularly susceptible to the effects of low testosterone levels. Research has shown that hypogonadal men often exhibit reduced pelvic floor EMG activity, which can contribute to issues like erectile dysfunction and urinary incontinence.
The Role of Hormone Replacement Therapy
Hormone replacement therapy, specifically testosterone replacement, has been a cornerstone in managing hypogonadism. By restoring testosterone levels to normal, HRT aims to alleviate symptoms and improve overall quality of life. Recent studies have focused on the specific impact of HRT on pelvic floor EMG activity, with promising results.
Study Findings on Pelvic Floor EMG Activity
A recent clinical study investigated the effects of targeted HRT on pelvic floor EMG activity in hypogonadal men. The study included a cohort of American males diagnosed with hypogonadism, who underwent a regimen of testosterone replacement over a six-month period. Baseline and follow-up EMG assessments were conducted to measure changes in pelvic floor muscle activity.
The results were striking. Participants showed a significant increase in pelvic floor EMG activity post-HRT, suggesting an improvement in muscle function. This enhancement in EMG activity correlated with self-reported improvements in urinary and sexual function, indicating a direct benefit of HRT on pelvic floor health.
Mechanisms Behind the Improvement
The improvement in pelvic floor EMG activity following HRT can be attributed to testosterone's anabolic effects on muscle tissue. Testosterone promotes protein synthesis and muscle growth, which likely contributes to the observed increase in muscle activity. Additionally, testosterone may enhance neuromuscular transmission, further supporting the functional improvement of the pelvic floor muscles.
Implications for American Males
For American males dealing with hypogonadism, these findings offer hope and a potential solution to pelvic floor-related issues. By addressing the underlying hormonal imbalance through HRT, men can experience not only a boost in overall well-being but also specific improvements in urinary and sexual function. It is crucial, however, for individuals to consult with healthcare providers to determine the appropriateness of HRT and to monitor its effects closely.
Future Directions in Research
While the current study provides valuable insights, further research is needed to fully understand the long-term effects of HRT on pelvic floor EMG activity. Future studies should explore different HRT regimens, the impact on various age groups, and potential side effects. Additionally, integrating other therapeutic modalities, such as pelvic floor exercises, could enhance the benefits of HRT.
Conclusion
The relationship between hypogonadism and pelvic floor EMG activity is a critical area of study, with significant implications for American males. Targeted hormone replacement therapy has shown promising results in improving pelvic floor muscle function, offering a potential pathway to better urinary and sexual health. As research continues to evolve, it is essential for men to stay informed and engage with healthcare professionals to optimize their treatment and quality of life.
Contact Us Today For A Free Consultation

- Testosterone's Impact on Bladder Health: Insights from Electron Microscopy Studies [Last Updated On: March 7th, 2025] [Originally Added On: March 7th, 2025]
- Understanding Urethral Epithelial Atrophy: Impact, Diagnosis, and Hormone Replacement Therapy [Last Updated On: March 8th, 2025] [Originally Added On: March 8th, 2025]
- Testosterone's Impact on Prostatic Stroma: Implications for Prostate Health and Therapy [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Exploring the Dynamics of Post-Void Residual Volume in Men with Testosterone Deficiency: A Longitudinal Study on Testosterone Replacement Therapy [Last Updated On: March 13th, 2025] [Originally Added On: March 13th, 2025]
Word Count: 576