Abstract:
Hormone Replacement Therapy (HRT) has long been a staple of medical practice for those seeking relief from the symptoms of hormone insufficiency or imbalance. The hormone testosterone, sometimes known as a male sexual hormone, is of special importance in HRT. This study article gives an in-depth examination of testosterone's involvement in HRT, highlighting its relevance in preserving secondary sex characteristics, investigating its antecedents, and outlining the advantages and potential hazards of testosterone treatment. We rely on scholarly research publications to back up our findings.
Introduction:
Hormone Replacement Therapy (HRT) entails administering hormones to people who have hormone shortages or imbalances. Testosterone, one of the key male sexual hormones, is crucial in HRT, particularly for transgender people who want to match their secondary sex characteristics with their gender identification. The purpose of this research is to investigate the science and practice of testosterone replacement therapy.
Testosterone and Secondary Sex Characteristics:
Secondary sex characteristics include a variety of morphological traits that clearly identify men from females within a specific species. In the context of humans, these qualities appear as a set of traits that undergo significant modifications as a result of sex hormones, with testosterone emerging as a key orchestrator of these changes in men.
Facial hair development, a deeper voice, increased muscular mass, and the creation of a male-pattern body fat distribution are among the most notable secondary sex characteristics directly affected by testosterone. These characteristics combined create the physical basis for individuals' perceptual and sociocultural classification as masculine. [1]
In the field of Hormone Replacement Therapy (HRT), testosterone plays a critical role, acting as a pharmacological instrument to aid in the acquisition of these masculine secondary sex characteristics in people who were assigned female at birth (AFAB). For these guys, whose gender identification is masculine, testosterone treatment becomes a critical method of reconciling their physical appearance with their interior sense of self.
The use of testosterone in HRT for AFAB patients provides a way to bridge the gap between their natural gender identification and physical appearance. Under medical care, these individuals can undergo significant modifications in their secondary sex characteristics, improving their congruence with their self-identified gender.
Testosterone: Male Hormones and Precursors to Testosterone
Testosterone is a member of the hormone family known as androgens, which are often colloquially referred to as male hormones due to their predominant role in masculinizing processes within the human body.
In 1979, a study was conducted to determine whether precursors to testosterone could exert some of its effects by stimulating guanylate cyclase, the enzyme that catalyzes the formation of cyclic GMP from GTP because cyclic GMP and testosterone appear to have similar actions. At a concentration of 1 microM, the precursors--progesterone, pregnenolone, 17 alpha-progesterone, 17 alpha-hydroxyprogesterone, androstenedione, and dehydroepiandrosterone--caused a 2- to 3 1/2-fold increase in guanylate cyclase activity in rat liver, kidney, skeletal muscle, and ventral prostate. These precursors are made from cholesterol, which has no influence on the function of guanylate cyclase. At 1 microM, testosterone, 19-nortestosterone, 17-methyltestosterone, and 5 alpha-dihydrotestosterone increased guanylate cyclase activity 2- to 5-fold. [2]
The creation of testosterone is a unique biochemical process that begins with a seemingly unrelated molecule: cholesterol. Cholesterol is a precursor to testosterone, along with some other steroid hormones. It is usually related to cardiovascular health. It is transformed into testosterone by a series of complicated enzymatic activities that occur sequentially in the testes' Leydig cells.
Testosterone Replacement Therapy (TRT):
TRT is a medical intervention that involves the delivery of exogenous testosterone to persons with clinically confirmed low testosterone levels. TRT is frequently used to treat hypogonadism or inadequate testosterone production. It can also be used in transgender healthcare to assist people in achieving desired secondary sex traits.
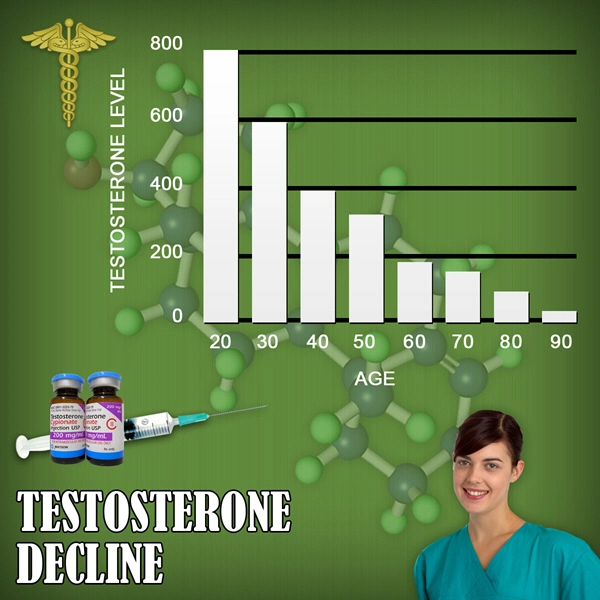
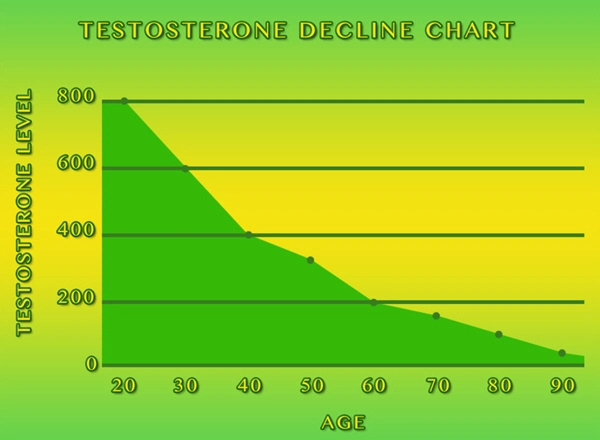
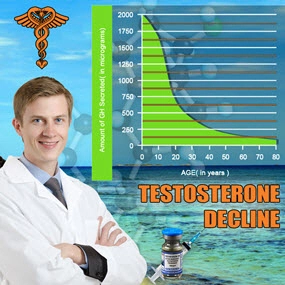
From early adulthood until old age, testosterone concentrations decrease in males. In T-Trials involving 788 men aged 65 years with baseline testosterone of 9.54 nmol/L, testosterone therapy for twelve months resulted in improvements in most aspects of sexual function, some benefits in mood and depressive symptoms, but not in vitality or cognition. [3]
Such significant test findings reveal various advantages, however small, from testosterone treatment in older men after 12 months, but further trials are needed to establish long-term health benefits and hazards.
Testosterone treatment for obesity leads to a minor increase in lean mass and a commensurate decrease in fat mass. Reducing excess weight, on the other hand, leads to significant increases in circulating testosterone concentrations proportional to the degree of weight reduction.
Testosterone treatment regularly and predictably heals symptoms of androgen insufficiency in males with pathological hypogonadism.
Benefits and Risks of Testosterone Therapy:
Testosterone therapy may have a wide range of deep and desirable impacts on the human body, affecting both physical and psychological elements of an individual's well-being. These effects include greater muscular growth, increased bone density, increased libido, and the development of masculine secondary sex traits.
In individuals undergoing gender transition or aligning their physical appearance with their gender identification, testosterone therapy can result in the development of masculine secondary sex characteristics. This includes characteristics such as increased facial hair development, a deeper voice, and a more male body fat distribution pattern. These changes are frequently profound for transgender people, matching their external appearance with their acknowledged gender identity and boosting their general quality of life.
Cardiovascular problems, mood changes, acne, and reproductive troubles are all potential side effects of testosterone treatment.
Conclusion:
Testosterone is essential in Hormone Replacement Therapy, particularly for those who want to match their secondary sex characteristics with their gender identification. Several studies have shed light on the importance of testosterone treatment in producing targeted physical changes.
Individuals seeking testosterone therapy should seek the advice of qualified medical experts who can give guidance, assess treatment progress, and handle possible dangers. The choice to use testosterone for HRT should be undertaken with informed consent and in conjunction with healthcare experts who are knowledgeable about transgender healthcare and endocrinology.
Our understanding of testosterone and its uses in HRT will surely develop as medical science advances, perhaps leading to even more effective and safer therapies for individuals wishing to control their secondary sex characteristics.
Contact Us Today For A Free Consultation

- Washington D.C. Testosterone Clinics for Low-T and Hormone Therapy [Last Updated On: October 1st, 2024] [Originally Added On: July 16th, 2018]
- Columbia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 2nd, 2024] [Originally Added On: November 11th, 2018]
- Charleston Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 14th, 2024] [Originally Added On: November 11th, 2018]
- Providence Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 24th, 2024] [Originally Added On: November 11th, 2018]
- Pittsburgh Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 7th, 2024] [Originally Added On: November 11th, 2018]
- Philadelphia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 15th, 2024] [Originally Added On: November 11th, 2018]
- Erie Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 22nd, 2024] [Originally Added On: November 11th, 2018]
- Allentown Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 10th, 2024] [Originally Added On: November 11th, 2018]
- Salem Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 6th, 2024] [Originally Added On: November 11th, 2018]
- Portland Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 11th, 2024] [Originally Added On: November 11th, 2018]
- Gresham Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 13th, 2024] [Originally Added On: November 11th, 2018]
- Eugene Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 19th, 2024] [Originally Added On: November 11th, 2018]
- Tulsa Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 13th, 2024] [Originally Added On: November 11th, 2018]
- Oklahoma City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 18th, 2024] [Originally Added On: November 11th, 2018]
- Norman Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 20th, 2024] [Originally Added On: November 11th, 2018]
- Toledo Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 21st, 2024] [Originally Added On: November 11th, 2018]
- Dayton Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 4th, 2024] [Originally Added On: November 11th, 2018]
- Columbus Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 24th, 2024] [Originally Added On: November 11th, 2018]
- Cleveland Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 12th, 2024] [Originally Added On: November 11th, 2018]
- Cincinnati Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 5th, 2024] [Originally Added On: November 11th, 2018]
- Akron Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 1st, 2024] [Originally Added On: November 11th, 2018]
- Bismarck Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 17th, 2024] [Originally Added On: November 11th, 2018]
- Winston-Salem Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 15th, 2024] [Originally Added On: November 11th, 2018]
- Wilmington Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 29th, 2024] [Originally Added On: November 11th, 2018]
- Raleigh Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 29th, 2024] [Originally Added On: November 11th, 2018]
- High Point Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 10th, 2024] [Originally Added On: November 11th, 2018]
- Greensboro Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 30th, 2024] [Originally Added On: November 11th, 2018]
- Fayetteville Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 19th, 2024] [Originally Added On: November 11th, 2018]
- Durham Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 24th, 2024] [Originally Added On: November 11th, 2018]
- Charlotte Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 7th, 2024] [Originally Added On: November 11th, 2018]
- Cary Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 16th, 2024] [Originally Added On: November 11th, 2018]
- Yonkers Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 7th, 2024] [Originally Added On: November 11th, 2018]
- Syracuse Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 10th, 2024] [Originally Added On: November 11th, 2018]
- Rochester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 16th, 2024] [Originally Added On: November 11th, 2018]
- Buffalo Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 5th, 2024] [Originally Added On: November 11th, 2018]
- Albuquerque Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 28th, 2024] [Originally Added On: November 11th, 2018]
- Paterson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 14th, 2024] [Originally Added On: November 11th, 2018]
- Newark Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 9th, 2024] [Originally Added On: November 11th, 2018]
- Jersey City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 19th, 2024] [Originally Added On: November 11th, 2018]
- Elizabeth Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 15th, 2024] [Originally Added On: November 11th, 2018]
- Manchester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 27th, 2024] [Originally Added On: November 11th, 2018]
- Reno Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 26th, 2024] [Originally Added On: November 11th, 2018]
- North Las Vegas Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 2nd, 2024] [Originally Added On: November 11th, 2018]
- Las Vegas Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 7th, 2024] [Originally Added On: November 11th, 2018]
- Henderson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 17th, 2024] [Originally Added On: November 11th, 2018]
- Omaha Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 17th, 2024] [Originally Added On: November 11th, 2018]
- Lincoln Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 30th, 2024] [Originally Added On: November 11th, 2018]
- Billings Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 8th, 2024] [Originally Added On: November 11th, 2018]
- St Louis Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 1st, 2024] [Originally Added On: November 11th, 2018]
- Springfield Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 1st, 2024] [Originally Added On: November 11th, 2018]
- Kansas City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 4th, 2024] [Originally Added On: November 11th, 2018]
- Independence Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 12th, 2024] [Originally Added On: November 11th, 2018]
- Columbia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 14th, 2024] [Originally Added On: November 11th, 2018]
- Jackson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 20th, 2024] [Originally Added On: November 11th, 2018]
- St Paul Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 12th, 2024] [Originally Added On: November 11th, 2018]
- Rochester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 3rd, 2024] [Originally Added On: November 11th, 2018]
- Minneapolis Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 6th, 2024] [Originally Added On: November 11th, 2018]
- Warren Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 10th, 2024] [Originally Added On: November 11th, 2018]
- Sterling Heights Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 13th, 2024] [Originally Added On: November 11th, 2018]
- Lansing Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 25th, 2024] [Originally Added On: November 11th, 2018]
- Grand Rapids Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 19th, 2024] [Originally Added On: November 11th, 2018]
- Flint Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 20th, 2024] [Originally Added On: November 11th, 2018]
- Detroit Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 23rd, 2024] [Originally Added On: November 11th, 2018]
- Ann Arbor Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 3rd, 2024] [Originally Added On: November 11th, 2018]
- Worcester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 28th, 2024] [Originally Added On: November 11th, 2018]
- Springfield Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 15th, 2024] [Originally Added On: November 11th, 2018]
- Lowell Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 25th, 2024] [Originally Added On: November 11th, 2018]
- Cambridge Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 6th, 2024] [Originally Added On: November 11th, 2018]
- Boston Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 16th, 2024] [Originally Added On: November 11th, 2018]
- Baltimore Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 7th, 2024] [Originally Added On: November 11th, 2018]
- Augusta Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 21st, 2024] [Originally Added On: November 11th, 2018]
- Shreveport Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 2nd, 2024] [Originally Added On: November 11th, 2018]
- New Orleans Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 16th, 2024] [Originally Added On: November 11th, 2018]
- Lafayette Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 24th, 2024] [Originally Added On: November 11th, 2018]
- Baton Rouge Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 2nd, 2024] [Originally Added On: November 11th, 2018]
- Louisville Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 23rd, 2024] [Originally Added On: November 11th, 2018]
- Lexington Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 11th, 2024] [Originally Added On: November 11th, 2018]
- Wichita Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 26th, 2024] [Originally Added On: November 11th, 2018]
- Topeka Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 28th, 2024] [Originally Added On: November 11th, 2018]
- Overland Park Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 20th, 2024] [Originally Added On: November 11th, 2018]
Word Count: 1006