The male hormone testosterone is required for a variety of physiological processes, including muscular growth, bone health, and overall well-being. Because it has been related to a variety of health issues in men, testosterone deficiency, also known as hypogonadism, is a disease characterized by lower-than-normal testosterone levels. The complicated link between low testosterone and male obesity, frailty, and multimorbidity is investigated in this study.
We look at the epidemiology, etiology, clinical symptoms, diagnostic criteria, and therapies for low testosterone. We also examine the accumulating evidence that testosterone deficiency weakens people and contributes to the formation of various comorbid disorders, emphasizing the need for early identification and treatment.
Introduction:
Testosterone is a critical hormone that governs a multitude of physiological processes in males, including muscular growth and strength, bone density, mood, and sexual function. It is primarily produced in the testes. Naturally, testosterone levels decline as men age, but in certain cases, the decline is substantial, resulting in hypogonadism or testosterone insufficiency. A variety of testosterone deficiency symptoms have been linked to an increased risk of a variety of disorders, including weakness and multimorbidity. The purpose of this research is to conduct an in-depth analysis of testosterone deficiency's prevalence, etiology, clinical consequences, and role in men's frailty and multimorbidity.
Age-Related Testosterone Deficiency in Men: Implications for Health and Well-being
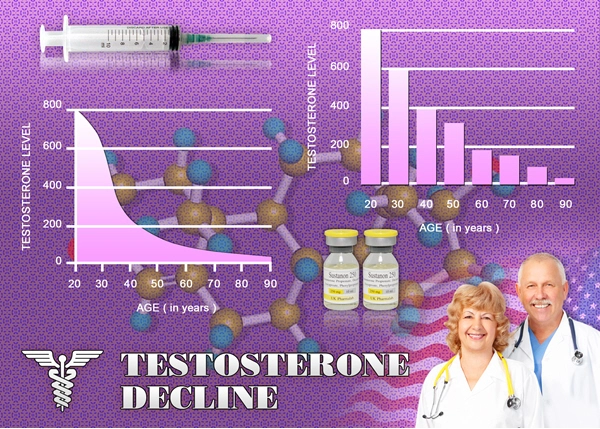
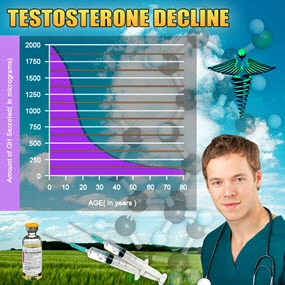
According to 2011 data, testosterone has become one of the most often prescribed drugs in the United States, with prescriptions growing fivefold. This development has resulted in a substantial expansion in the pharmaceutical industry's testosterone replacement treatment (TRT) sector, which has grown from US$18 million in the 1980s to US$1.6 billion in 2011. The explanation is numerous, but it may be linked in part to the ongoing rise of the over-65 population and a growing awareness of medical comorbidities associated with low testosterone, such as metabolic syndrome (MetS) and cardiovascular disease (CVD). [1]
After age 30, testosterone levels start to drop quickly (by up to 2% yearly), with 35% of men in their seventh decade having lower testosterone levels than younger men and 13% of men over the age of 60 meeting the diagnostic criteria for hypogonadism. This has caused a subset of men with hypogonadism, known as "late-onset" hypogonadism (LOH) or andropause, to develop who are older than 65 years old.
Male adult reproductive health, sexual function, bone health, fat metabolism, and muscular mass and strength are all significantly influenced by testosterone. The hypothalamic-pituitary-gonadal (HPG) axis tightly controls the synthesis of testosterone by testicular Leydig cells through the release of luteinizing hormone (LH). Primary, secondary, or mixed hypogonadism can develop from failure to maintain this delicate equilibrium.
Due to a variety of factors, the prevalent type of testosterone deficiency (TD) in older men combines elements of primary and secondary hypogonadism. LH levels in elderly men might fluctuate depending on factors such as decreasing Leydig cell numbers and function, decreased HPG axis sensitivity to feedback inhibition, and/or lower LH pulse amplitude despite normal pulse frequency.
Diagnostic Criteria for Testosterone Deficiency:
Due to the absence of high-quality, randomized studies in older men, the diagnosis of TD in aging men is predicated on the presence of both clinical symptoms and low blood testosterone levels, similar to the method employed in younger or middle-aged men. However, due to the prevalence of symptoms related to normal aging that coincide with those associated with TD, diagnosing TD in older males is more challenging. However, due to the obvious age-related decline in testosterone levels, assessing individuals for biochemical TD alone might result in a considerable overdiagnosis.
In actuality, many older men with 'low testosterone' don't even exhibit any symptoms. Due to this conundrum, several influential medical associations and organizations have defined LOH as a clinical and biochemical condition that is linked to aging, manifested by symptoms, and characterized by blood testosterone levels below those of young, healthy guys. Due to these factors, during the first examination, specified etiologies of primary and secondary symptomatic hypogonadism must be distinguished from LOH; otherwise, the apparent low testosterone may just be a normal physiological reaction to age.
Laboratory testing is necessary to confirm the diagnosis of hypogonadism in older men who exhibit its signs or symptoms. Due to diurnal variance, initial testing should include a total blood testosterone level collected between 7 a.m. and 11 a.m. However, a considerable percentage of older men might experience blunting of the diurnal fluctuation, and up to 30% of individuals with initially abnormal findings will have normal levels on subsequent testing. [2]
Multimorbidity:
According to Pearson-Stuttard et al. (2019), one of the biggest current and upcoming issues for healthcare systems is multimorbidity. However, the definition of the word "multimorbidity" is still up for debate. [3]
The phrase evokes a wide range of interpretations, including but not limited to:
- the coexistence of several aging-related health issues among older persons, which is linked to (and implicitly caused by) an aging global population;
- The early development and widespread occurrence of complicated, long-term mental and physical health disorders that are made worse by unfavorable socioeconomic circumstances. This type of multimorbidity emphasizes how disease and societal hardship reinforce one another;
- The co-existence of two or more chronic illnesses in one individual whose demands are not completely satisfied by care systems that are set up on a "single disease" approach. Multimorbidity is not seen as a stable entity in this theory but rather as an "avatar for the fundamental, recurring problems of modern medicine and the organization of care," according to Lefèvre and colleagues.
Conclusion:
The complicated and multidimensional illness of testosterone shortage can significantly affect the health and well-being of men. It is linked to a variety of testosterone deficiency symptoms, such as mood swings, sexual dysfunction, and physical weakness. A lack of testosterone may also lead to the emergence of multimorbidity, which includes cardiovascular disease, metabolic syndrome, obesity, type 2 diabetes, and osteoporosis, according to new research.
To lessen the symptoms of testosterone insufficiency and enhance the general health and quality of life of afflicted people, early identification and adequate care of the condition are crucial. Clinicians should carefully assess patients who exhibit signs of low testosterone while taking into account the possible advantages and disadvantages of testosterone replacement treatment on an individual basis. To completely understand the intricate interactions between low testosterone and multimorbidity and to improve therapy approaches for this illness, more study is required.
Contact Us Today For A Free Consultation

- Washington D.C. Testosterone Clinics for Low-T and Hormone Therapy [Last Updated On: October 1st, 2024] [Originally Added On: July 16th, 2018]
- Columbia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 2nd, 2024] [Originally Added On: November 11th, 2018]
- Charleston Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 14th, 2024] [Originally Added On: November 11th, 2018]
- Providence Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 24th, 2024] [Originally Added On: November 11th, 2018]
- Pittsburgh Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 7th, 2024] [Originally Added On: November 11th, 2018]
- Philadelphia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 15th, 2024] [Originally Added On: November 11th, 2018]
- Erie Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 22nd, 2024] [Originally Added On: November 11th, 2018]
- Allentown Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 10th, 2024] [Originally Added On: November 11th, 2018]
- Salem Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 6th, 2024] [Originally Added On: November 11th, 2018]
- Portland Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 11th, 2024] [Originally Added On: November 11th, 2018]
- Gresham Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 13th, 2024] [Originally Added On: November 11th, 2018]
- Eugene Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 19th, 2024] [Originally Added On: November 11th, 2018]
- Tulsa Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 13th, 2024] [Originally Added On: November 11th, 2018]
- Oklahoma City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 18th, 2024] [Originally Added On: November 11th, 2018]
- Norman Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 20th, 2024] [Originally Added On: November 11th, 2018]
- Toledo Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 21st, 2024] [Originally Added On: November 11th, 2018]
- Dayton Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 4th, 2024] [Originally Added On: November 11th, 2018]
- Columbus Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 24th, 2024] [Originally Added On: November 11th, 2018]
- Cleveland Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 12th, 2024] [Originally Added On: November 11th, 2018]
- Cincinnati Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 5th, 2024] [Originally Added On: November 11th, 2018]
- Akron Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 1st, 2024] [Originally Added On: November 11th, 2018]
- Bismarck Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 17th, 2024] [Originally Added On: November 11th, 2018]
- Winston-Salem Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 15th, 2024] [Originally Added On: November 11th, 2018]
- Wilmington Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 29th, 2024] [Originally Added On: November 11th, 2018]
- Raleigh Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 29th, 2024] [Originally Added On: November 11th, 2018]
- High Point Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 10th, 2024] [Originally Added On: November 11th, 2018]
- Greensboro Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 30th, 2024] [Originally Added On: November 11th, 2018]
- Fayetteville Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 19th, 2024] [Originally Added On: November 11th, 2018]
- Durham Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 24th, 2024] [Originally Added On: November 11th, 2018]
- Charlotte Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 7th, 2024] [Originally Added On: November 11th, 2018]
- Cary Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 16th, 2024] [Originally Added On: November 11th, 2018]
- Yonkers Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 7th, 2024] [Originally Added On: November 11th, 2018]
- Syracuse Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 10th, 2024] [Originally Added On: November 11th, 2018]
- Rochester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 16th, 2024] [Originally Added On: November 11th, 2018]
- Buffalo Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 5th, 2024] [Originally Added On: November 11th, 2018]
- Albuquerque Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 28th, 2024] [Originally Added On: November 11th, 2018]
- Paterson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 14th, 2024] [Originally Added On: November 11th, 2018]
- Newark Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 9th, 2024] [Originally Added On: November 11th, 2018]
- Jersey City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 19th, 2024] [Originally Added On: November 11th, 2018]
- Elizabeth Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 15th, 2024] [Originally Added On: November 11th, 2018]
- Manchester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 27th, 2024] [Originally Added On: November 11th, 2018]
- Reno Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 26th, 2024] [Originally Added On: November 11th, 2018]
- North Las Vegas Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 2nd, 2024] [Originally Added On: November 11th, 2018]
- Las Vegas Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 7th, 2024] [Originally Added On: November 11th, 2018]
- Henderson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 17th, 2024] [Originally Added On: November 11th, 2018]
- Omaha Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 17th, 2024] [Originally Added On: November 11th, 2018]
- Lincoln Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 30th, 2024] [Originally Added On: November 11th, 2018]
- Billings Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 8th, 2024] [Originally Added On: November 11th, 2018]
- St Louis Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 1st, 2024] [Originally Added On: November 11th, 2018]
- Springfield Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 1st, 2024] [Originally Added On: November 11th, 2018]
- Kansas City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 4th, 2024] [Originally Added On: November 11th, 2018]
- Independence Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 12th, 2024] [Originally Added On: November 11th, 2018]
- Columbia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 14th, 2024] [Originally Added On: November 11th, 2018]
- Jackson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 20th, 2024] [Originally Added On: November 11th, 2018]
- St Paul Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 12th, 2024] [Originally Added On: November 11th, 2018]
- Rochester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 3rd, 2024] [Originally Added On: November 11th, 2018]
- Minneapolis Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 6th, 2024] [Originally Added On: November 11th, 2018]
- Warren Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 10th, 2024] [Originally Added On: November 11th, 2018]
- Sterling Heights Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 13th, 2024] [Originally Added On: November 11th, 2018]
- Lansing Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 25th, 2024] [Originally Added On: November 11th, 2018]
- Grand Rapids Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 19th, 2024] [Originally Added On: November 11th, 2018]
- Flint Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 20th, 2024] [Originally Added On: November 11th, 2018]
- Detroit Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 23rd, 2024] [Originally Added On: November 11th, 2018]
- Ann Arbor Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 3rd, 2024] [Originally Added On: November 11th, 2018]
- Worcester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 28th, 2024] [Originally Added On: November 11th, 2018]
- Springfield Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 15th, 2024] [Originally Added On: November 11th, 2018]
- Lowell Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 25th, 2024] [Originally Added On: November 11th, 2018]
- Cambridge Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 6th, 2024] [Originally Added On: November 11th, 2018]
- Boston Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 16th, 2024] [Originally Added On: November 11th, 2018]
- Baltimore Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 7th, 2024] [Originally Added On: November 11th, 2018]
- Augusta Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 21st, 2024] [Originally Added On: November 11th, 2018]
- Shreveport Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 2nd, 2024] [Originally Added On: November 11th, 2018]
- New Orleans Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 16th, 2024] [Originally Added On: November 11th, 2018]
- Lafayette Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 24th, 2024] [Originally Added On: November 11th, 2018]
- Baton Rouge Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 2nd, 2024] [Originally Added On: November 11th, 2018]
- Louisville Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 23rd, 2024] [Originally Added On: November 11th, 2018]
- Lexington Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 11th, 2024] [Originally Added On: November 11th, 2018]
- Wichita Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 26th, 2024] [Originally Added On: November 11th, 2018]
- Topeka Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 28th, 2024] [Originally Added On: November 11th, 2018]
- Overland Park Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 20th, 2024] [Originally Added On: November 11th, 2018]
Word Count: 1049