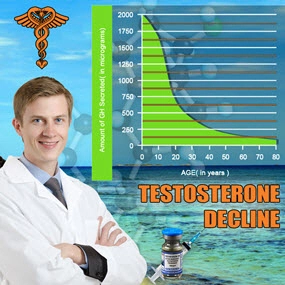
Introduction to Low Testosterone and Chronic Illness
Low testosterone, medically known as hypogonadism, is a condition that affects a significant number of American males, leading to a variety of symptoms including decreased libido, fatigue, and mood disturbances. Chronic illnesses, which are long-lasting health conditions, can further complicate this scenario by directly influencing testosterone production and metabolism. Understanding the relationship between chronic illness and low testosterone levels is crucial for effective management and treatment.
The Physiology of Testosterone and Its Regulation
Testosterone, the primary male sex hormone, is produced mainly in the testicles and is essential for the development of male reproductive tissues and secondary sexual characteristics. Its production is regulated by the hypothalamic-pituitary-gonadal (HPG) axis, which can be disrupted by various chronic conditions. Diseases such as diabetes, obesity, and chronic kidney disease are known to interfere with this axis, leading to reduced testosterone levels.
Diabetes and Testosterone Levels
Diabetes mellitus, a prevalent chronic illness in the United States, has a well-documented association with low testosterone. The metabolic disturbances caused by diabetes, such as insulin resistance, can impair the function of the Leydig cells in the testes, which are responsible for testosterone production. Studies have shown that men with type 2 diabetes are at a higher risk of developing hypogonadism, which can exacerbate the symptoms of diabetes and complicate its management.
Obesity's Role in Testosterone Reduction
Obesity, another common chronic condition among American males, is closely linked to low testosterone levels. Adipose tissue, or body fat, can convert testosterone into estradiol, a form of estrogen, through the action of the enzyme aromatase. This conversion leads to a decrease in circulating testosterone. Furthermore, obesity can lead to insulin resistance and inflammation, both of which can negatively impact testosterone production.
Chronic Kidney Disease and Hormonal Imbalance
Chronic kidney disease (CKD) is another significant factor that can lead to low testosterone levels. The kidneys play a crucial role in the metabolism and clearance of hormones, and their dysfunction can lead to hormonal imbalances. CKD can also cause anemia, which is associated with low testosterone levels. Additionally, the treatment modalities for CKD, such as dialysis, can further influence testosterone levels, making it a complex interplay that requires careful management.
The Psychological Impact of Low Testosterone
Beyond the physical symptoms, low testosterone can have profound psychological effects. Chronic illnesses can exacerbate these effects, leading to a vicious cycle of worsening health. Depression, anxiety, and reduced quality of life are common in men with low testosterone, and these symptoms can be intensified by the presence of chronic conditions. Addressing both the hormonal and psychological aspects is essential for comprehensive care.
Management and Treatment Strategies
The management of low testosterone in the context of chronic illness involves a multifaceted approach. Hormone replacement therapy (HRT) can be considered, but it must be tailored to the individual's overall health status and the specific chronic conditions they are managing. Lifestyle modifications, such as weight loss and improved diet, can also play a significant role in improving testosterone levels and overall health. Regular monitoring and a collaborative approach between endocrinologists, primary care physicians, and other specialists are crucial for optimizing outcomes.
Conclusion: A Holistic Approach to Low Testosterone and Chronic Illness
The interplay between chronic illness and low testosterone in American males is a complex issue that requires a holistic approach to management. By understanding the physiological mechanisms and the impact of specific chronic conditions, healthcare providers can develop targeted strategies to improve testosterone levels and enhance the quality of life for affected individuals. Continued research and awareness are essential to advance our understanding and treatment of this prevalent health concern.
Contact Us Today For A Free Consultation

- Environmental Toxins and Testosterone: Impacts and Mitigation Strategies for American Men [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Low Testosterone in American Males: Symptoms, Causes, and Treatment Options [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Low Testosterone's Impact on Muscle Mass and Strength in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Vitamin D's Role in Managing Low Testosterone in American Men: A Comprehensive Review [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
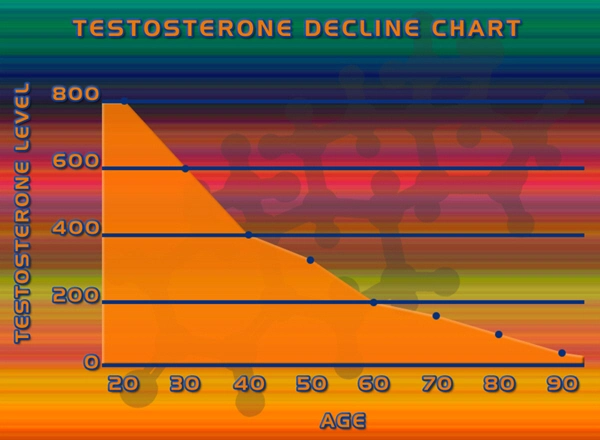
- Managing Low Testosterone in Aging Men: Symptoms, Treatments, and Lifestyle Strategies [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Economic Burden of Low Testosterone on American Healthcare System [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Low Testosterone and Diabetes: Dual Challenges Impacting American Men's Health [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Alcohol Consumption and Its Impact on Testosterone Levels in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Zinc's Role in Boosting Testosterone Levels in American Men: A Comprehensive Review [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Low Testosterone and Mood Disorders: Impact and Management in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Low Testosterone in American Men: Symptoms, Diagnosis, and Treatment Strategies [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Smoking's Impact on Testosterone Levels in American Men: Risks and Recovery [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Low Testosterone's Impact on Osteoporosis Risk in American Men: Detection and Management [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone and Prostate Health: Risks, Therapy, and Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone and Hair Loss: Understanding the Link and Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone's Impact on Cognitive Function in American Men: Insights and Interventions [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Shift Work's Impact on Testosterone Levels in American Men: Health Implications and Mitigation [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone's Impact on Immune Health in American Males: Insights and Management [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Optimizing Testosterone Levels: Dietary Strategies for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Low Testosterone in American Men: Symptoms, Impact, and Treatment Options [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Environmental Estrogens: A Hidden Cause of Low Testosterone in American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Low Testosterone's Impact on Skin Health in American Men: Causes and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Weight Loss Boosts Testosterone: A Guide for American Males with Low T [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Herbal Supplements for Low Testosterone: Benefits, Limitations, and Efficacy in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Managing Low Testosterone in Aging Men: Symptoms, Treatments, and Lifestyle Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone and Heart Disease: Risks, Mechanisms, and Management in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Chronic Stress Impact on Testosterone Levels in American Men: Causes and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone's Impact on Emotional Wellbeing in American Men: Insights and Guidance [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone and Depression: Understanding the Link and Its Impact on American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Sleep Apnea's Impact on Testosterone Levels in American Males: Insights and Solutions [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Medications Impacting Testosterone Levels: Insights for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone and Metabolic Syndrome: Implications for American Men's Health [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Chronic Pain's Impact on Testosterone Levels in American Males: A Comprehensive Analysis [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Genetic Factors in Low Testosterone Among American Males: Insights and Implications [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone Linked to Increased Thyroid Disorder Risk in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone and Insulin Resistance: Exploring the Link in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Exercise Boosts Testosterone: A Guide for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone and Libido: Impacts, Diagnosis, and Treatment for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone's Impact on Body Composition in American Males: Challenges and Management [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Low Testosterone and Skin Health: Dermatological Impacts and Management in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Chronic Inflammation and Low Testosterone: Strategies for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Nutrition's Impact on Testosterone: Deficiencies and Dietary Solutions for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Respiratory Health's Impact on Testosterone Levels in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone's Role and Managing Low Levels in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Low Testosterone Linked to Anemia Risk in American Men: Insights and Management [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Low Testosterone Linked to Autoimmune Diseases in American Men: Insights and Management [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Liver Health Crucial for Testosterone Balance in American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Gut Health and Testosterone: Optimizing Hormonal Balance in American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Low Testosterone Linked to Increased Kidney Disease Risk in American Men [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Low Testosterone Linked to Neurological Risks in American Men: Implications and Interventions [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
Word Count: 598