Introduction
Andropause, colloquially known as "male menopause," is a term used to describe the gradual decline in testosterone levels in aging men. This physiological transition has been the subject of extensive research over the past two decades, particularly in relation to its impact on prostate health and the risk of developing prostate cancer. This article delves into the intricate relationship between andropause and prostate health in American males, exploring the latest findings and their implications for preventive healthcare.
Understanding Andropause
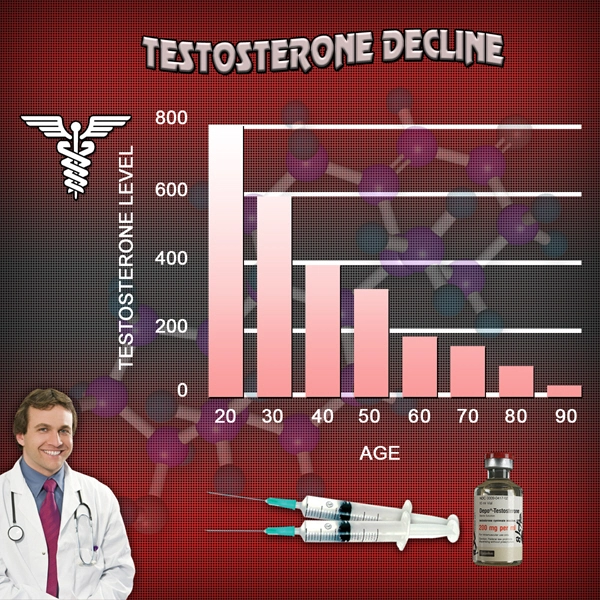
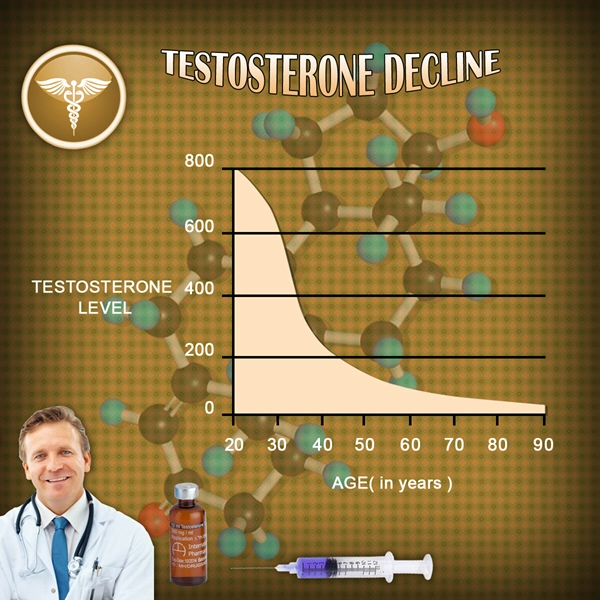
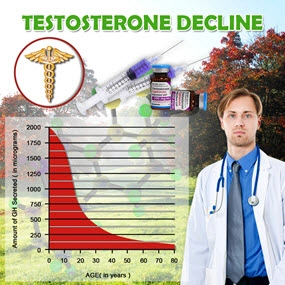
Andropause is characterized by a slow but steady decline in testosterone production, which typically begins in a man's late 30s to early 40s. Unlike the more abrupt hormonal changes experienced by women during menopause, andropause is a subtler process, often going unnoticed until symptoms become more pronounced. Symptoms may include decreased libido, fatigue, depression, and reduced muscle mass. The impact of these hormonal shifts on overall health, particularly prostate health, has been a focal point of medical research.
The Prostate and Hormonal Influence
The prostate gland, a crucial component of the male reproductive system, is highly sensitive to hormonal fluctuations. Testosterone and its metabolite, dihydrotestosterone (DHT), play significant roles in prostate function and growth. As men age and testosterone levels decline, the balance between testosterone and estrogen shifts, potentially influencing prostate health. Research over the past 20 years has sought to understand how these hormonal changes correlate with the development of prostate diseases, including benign prostatic hyperplasia (BPH) and prostate cancer.
Andropause and Prostate Cancer Risk
A comprehensive analysis of data spanning two decades reveals a complex relationship between andropause and prostate cancer risk. Early studies suggested that lower testosterone levels might be protective against prostate cancer, as testosterone is known to fuel prostate cell growth. However, more recent research has challenged this notion, indicating that the relationship may be more nuanced.
Key Findings from Longitudinal Studies
Longitudinal studies have shown that while low testosterone levels may initially appear protective, the risk of aggressive prostate cancer can increase in men with very low testosterone levels. This paradox suggests that maintaining a balanced hormonal milieu is crucial for prostate health. Furthermore, the role of estrogen, which increases relative to testosterone during andropause, has been implicated in promoting prostate cancer cell proliferation.
Implications for Preventive Healthcare
The insights gained from 20 years of research underscore the importance of monitoring hormonal health in aging American males. Regular screening for testosterone levels, coupled with prostate-specific antigen (PSA) tests, can help identify men at higher risk of developing prostate cancer. Additionally, lifestyle interventions that promote hormonal balance, such as maintaining a healthy weight, regular exercise, and a balanced diet, are recommended to mitigate the risks associated with andropause.
Future Directions in Research
As the medical community continues to unravel the complexities of andropause and its impact on prostate health, future research will likely focus on personalized medicine approaches. Tailoring interventions based on individual hormonal profiles and genetic predispositions could revolutionize the prevention and treatment of prostate cancer. Moreover, ongoing studies aim to better understand the role of other hormones, such as insulin-like growth factor (IGF-1), in the development of prostate diseases.
Conclusion
The relationship between andropause and prostate health in American males is a multifaceted issue that has evolved significantly over the past 20 years. While the decline in testosterone associated with andropause presents challenges, it also offers opportunities for early intervention and preventive care. By staying informed about the latest research and adopting a proactive approach to health, American males can better navigate the complexities of aging and maintain optimal prostate health.
Contact Us Today For A Free Consultation

- Understanding Andropause: Male Menopause, Symptoms, and Management Strategies [Last Updated On: March 7th, 2025] [Originally Added On: March 7th, 2025]
- Andropause in American Males: Myths, Realities, and Management Strategies [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Andropause in American Men: Supplements and Holistic Management Strategies [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Managing Andropause: Diet, Exercise, Stress, and Hormone Therapy Strategies for American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Navigating Andropause: Understanding Emotional Changes and Support Strategies for Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Andropause and Depression: Symptoms, Interventions, and Empowerment for American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Andropause: Embracing Male Menopause as a Growth Opportunity for American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Andropause Management: Importance of Regular Check-ups for American Men's Health [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Andropause and Diabetes Risk in American Males: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Andropause and Prostate Health: Understanding the Link and Managing Symptoms [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Managing Andropause: Boosting Energy and Vitality in American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Andropause and Cognitive Health: Strategies for American Men to Maintain Mental Sharpness [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Andropause: Managing Emotional Well-being in American Men Through Diet, Exercise, and Support [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Andropause: Navigating Social Impacts and Coping Strategies for American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Andropause: Building Support Networks for American Men's Health and Well-being [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Andropause Effects on Skin: Understanding and Managing Changes in Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Andropause and Hair Loss: Understanding Causes and Exploring Treatment Options [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Andropause: Mental Health Professionals' Role in Managing Psychological Impact [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Managing Andropause: A Guide for American Males to Discuss with Healthcare Providers [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Andropause and Digestive Health: Strategies for American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hydration's Crucial Role in Managing Andropause Symptoms and Enhancing Well-being [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Andropause in American Males: Managing Muscle Loss and Health [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Andropause: Understanding Male Menopause and Its Impact on Energy Levels in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Andropause: Understanding and Managing Male Menopause Effects on American Men's Lives [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Andropause in American Men: Enhancing Sleep Quality for Symptom Management [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Andropause Impact on Kidney Health: Symptoms, Management, and Monitoring for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Andropause and Joint Health: Strategies for American Men to Maintain Vitality [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Andropause and Memory: Strategies for Enhancing Recall in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Andropause: Exercise Benefits and Strategies for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Andropause: Stress Reduction Techniques for American Men's Health [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Andropause and Liver Health: Impacts and Management Strategies for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Andropause and Cholesterol: Management Strategies for Aging American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Managing Andropause: Importance of Screenings and Lifestyle Changes for Men's Health [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Andropause and Thyroid Function: Impacts and Management in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Andropause and Vision: Managing Eye Health in Aging American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Andropause: Understanding and Managing Declining Motivation in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Andropause Management: Benefits and Risks of Hormone Replacement Therapy for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Managing Andropause: Nutrition and Lifestyle Strategies for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Understanding Andropause: Symptoms, Causes, and Management for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Andropause: Understanding Male Menopause and the Importance of Community Support [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Andropause: Managing Symptoms and Balancing Work-Life for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause and Self-Esteem: Impacts and Management Strategies for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause: Managing Mental Health and Breaking Stigma in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause and Emotional Intelligence: Navigating Challenges for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause and Respiratory Health: Symptoms, Links, and Management Strategies for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Mindfulness: A Holistic Approach to Managing Andropause Symptoms in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause: Understanding Male Menopause and Its Impact on American Men's Confidence [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause and Immune Health: Strategies for American Males to Boost Well-being [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause: Understanding Symptoms, Family Support, and Healthy Lifestyle Changes for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Andropause and Blood Pressure: Monitoring and Management Tips for American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Andropause and Hearing Loss: Understanding the Link in American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Andropause and Dental Health: Essential Tips for American Males [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Hobbies: A Vital Tool for Managing Andropause in American Men [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Andropause in American Men: Impact on Creativity and Mitigation Strategies [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Andropause and Allergies: Managing Symptoms and Improving Quality of Life in American Males [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Navigating Andropause: Setting Goals for Health, Career, and Relationships [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Andropause: Managing Time Effectively to Enhance Life Quality in Aging American Men [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Andropause: Navigating Male Menopause and Its Impact on American Men's Lives [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Andropause Impact on Foot Health: Prevention and Management for American Males [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Andropause and Lifelong Learning: Enhancing Life Quality for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Technology's Role in Managing Andropause for American Men: Wearables to Digital Therapeutics [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Andropause Effects on Hand Health: Symptoms, Management for American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Volunteering: A Holistic Approach to Managing Andropause in American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Andropause and Skin Sensitivity: Managing Symptoms in American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Andropause: Understanding Its Impact on American Men's Adventurous Spirit [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Andropause and Eye Health: Impacts and Management for American Males [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Andropause Effects on Nail Health: Nutritional and Lifestyle Strategies for American Men [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Travel as Therapy: Managing Andropause in American Men [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Andropause and Nasal Health: Understanding the Link and Managing Symptoms in American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Andropause: Understanding Testosterone Decline and Its Impact on Men's Humor and Well-being [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Andropause Impact on Throat Health: Strategies for American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Music Therapy: A Holistic Approach to Managing Andropause Symptoms in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Andropause: Financial Planning Strategies for American Men's Health and Retirement [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Andropause Effects on Oral Health: Understanding Tongue Changes and Management Strategies [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Art Therapy: A Holistic Approach to Managing Andropause in American Men [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Andropause: Navigating Testosterone Decline and Identity in American Men [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Andropause in American Men: Navigating Social Isolation and Building Connections [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Andropause Effects on Ear Health: Strategies for American Males [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Andropause and Cognitive Decline: Insights from a 20-Year Study on American Men [Last Updated On: April 23rd, 2025] [Originally Added On: April 23rd, 2025]
- 20-Year Study Reveals Andropause's Impact on Employment, Income, and Quality of Life in American Males [Last Updated On: April 23rd, 2025] [Originally Added On: April 23rd, 2025]
Word Count: 585