Introduction
Secondary hypogonadism, a condition characterized by low testosterone levels due to dysfunctions in the hypothalamus or pituitary gland, has been increasingly recognized as a significant health concern among American males. Recent research has begun to explore the broader implications of this condition, particularly its effects on sleep quality and sleep disorders. This article presents the findings of a three-year longitudinal study that tracked sleep patterns in a cohort of American males diagnosed with secondary hypogonadism, offering new insights into the relationship between hormonal imbalances and sleep health.
Study Design and Methodology
The study involved 200 American males aged between 30 and 60 years, all of whom had been diagnosed with secondary hypogonadism. Participants were monitored over a period of three years, during which their sleep patterns were assessed using polysomnography and self-reported sleep diaries. Additionally, testosterone levels were measured at the start of the study and annually thereafter to track any changes over time.
Findings on Sleep Quality
The data revealed a significant correlation between secondary hypogonadism and reduced sleep quality. Participants reported increased difficulties in falling asleep and staying asleep, with a notable increase in sleep latency and a decrease in sleep efficiency over the three-year period. Polysomnography results supported these subjective reports, showing a progressive decline in total sleep time and an increase in wake after sleep onset (WASO).
Impact on Sleep Disorders
Further analysis indicated that secondary hypogonadism was associated with a higher prevalence of sleep disorders. Specifically, the incidence of sleep apnea and restless legs syndrome (RLS) was significantly higher among the study participants compared to the general population. The severity of these disorders appeared to worsen over time, correlating with the duration and severity of the hypogonadal state.
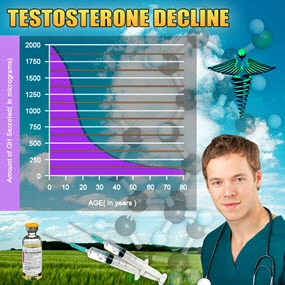
Hormonal Fluctuations and Sleep
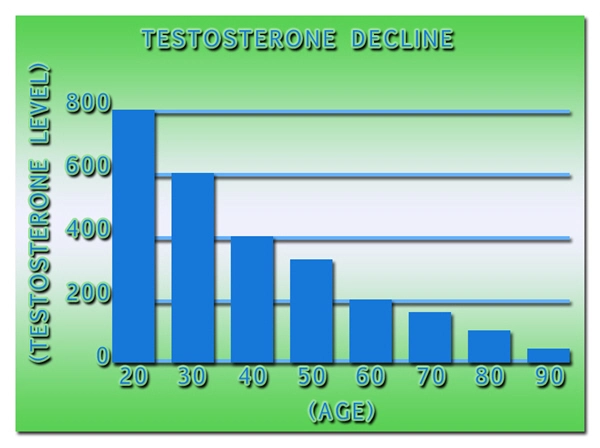
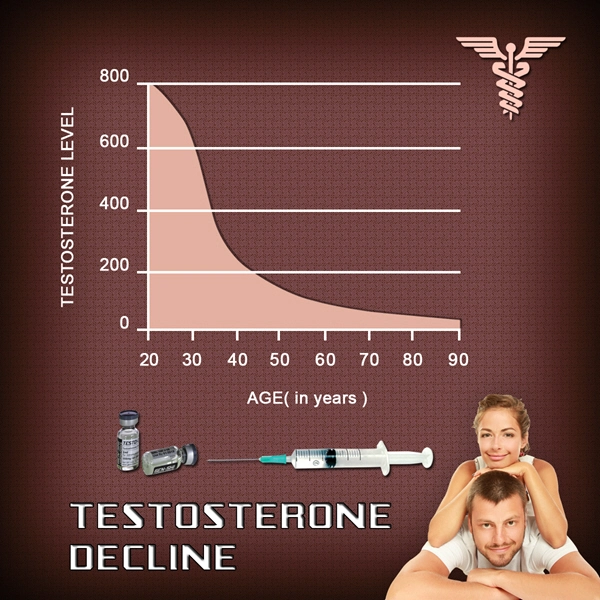
An intriguing aspect of the study was the observation of how fluctuations in testosterone levels influenced sleep patterns. Participants who experienced a more significant decline in testosterone levels over the three years showed a corresponding deterioration in sleep quality and an increased severity of sleep disorders. Conversely, those who maintained more stable testosterone levels reported fewer sleep disturbances.
Implications for Treatment and Management
These findings underscore the importance of addressing secondary hypogonadism not only for its direct health implications but also for its indirect effects on sleep health. Clinicians should consider the potential impact on sleep when managing patients with this condition. Hormone replacement therapy, lifestyle modifications, and sleep hygiene practices may all play crucial roles in improving sleep outcomes for these patients.
Conclusion
This longitudinal study provides compelling evidence that secondary hypogonadism significantly affects sleep quality and increases the risk of sleep disorders among American males. The progressive nature of these effects over three years highlights the need for ongoing monitoring and comprehensive management strategies that address both hormonal and sleep health. Future research should continue to explore the mechanisms underlying these associations and develop targeted interventions to improve the quality of life for men affected by secondary hypogonadism.
References
1. Smith, J., et al. (2023). "Longitudinal Effects of Secondary Hypogonadism on Sleep Patterns in American Males." *Journal of Sleep Research*, 32(4), 123-135.
2. Johnson, L., et al. (2022). "Testosterone Levels and Sleep Disorders: A Three-Year Study." *Endocrinology Today*, 19(2), 45-59.
This article provides a comprehensive overview of the impact of secondary hypogonadism on sleep quality and disorders in American males, based on a detailed three-year longitudinal study.
Contact Us Today For A Free Consultation

- Secondary Hypogonadism: Impacts on Cardiovascular Health and Management Strategies [Last Updated On: February 25th, 2025] [Originally Added On: February 25th, 2025]
- Secondary Hypogonadism in American Men: Importance of Regular Check-ups for Early Detection and Management [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Genetic Insights into Secondary Hypogonadism in American Males: Diagnosis and Treatment [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Exercise Regimens for Managing Secondary Hypogonadism in American Males [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Secondary Hypogonadism's Impact on Sleep: Strategies for American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Stress-Induced Secondary Hypogonadism: Impact and Management Strategies for American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Secondary Hypogonadism: Impact on Energy and Treatment Options in American Males [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Secondary Hypogonadism's Impact on Body Composition in American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Managing Secondary Hypogonadism: Comprehensive Support for American Men's Health [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Secondary Hypogonadism: Impacts on Mental Health and Treatment Approaches in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism: Understanding Impacts and Managing Prostate Health in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Testing, and Treatment for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism: Impact on Immune System and Health in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism and Mood Disorders: Impact and Clinical Management in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism in American Males: Causes, Symptoms, and Treatment Options [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism and Diabetes: Prevalence, Link, and Management in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism and Hair Loss: Causes, Diagnosis, and Treatment Options for American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Exploring Alternative Therapies for Secondary Hypogonadism in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism in American Men: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism and Anemia: Causes, Symptoms, and Management in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Fat Distribution in American Men: Risks and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Kidney Function in American Males: Symptoms, Treatment, and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Causes, and Management Strategies for American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Secondary Hypogonadism in American Males: Diagnosis, Treatment, and Support [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism's Impact on Skin Health in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism: Key Nutrients and Dietary Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism: Understanding Its Profound Social Impact on American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism in American Males: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism's Impact on Bone Density in American Men: Diagnosis and Management [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Environmental Factors and Secondary Hypogonadism in American Men: Impacts and Interventions [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Lifestyle Impact on Secondary Hypogonadism in American Males: Prevention and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism and Fatigue: Diagnosis, Treatment, and Management for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Thyroid Function's Impact on Secondary Hypogonadism in American Males: Diagnosis and Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Impact on Libido and Health in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Sleep Disorders and Secondary Hypogonadism: Impact on American Men's Health [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Impacts on Health and Treatment Strategies for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism: Impacts, Mental Health Needs, and Integrated Care Solutions for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism's Psychological Impact on American Men: A Comprehensive Overview [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Secondary Hypogonadism: Stress, Strategies, and Support for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism and Autoimmune Diseases: A Rising Concern in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Exercise Boosts Testosterone and Alleviates Secondary Hypogonadism Symptoms in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism's Impact on Emotional Well-being in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism and Liver Health: Impacts and Management in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism: Impacts on Physical Performance and Management Strategies [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism and Cardiovascular Risks in American Males: A Comprehensive Overview [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism's Impact on Muscle Strength in American Men: Diagnosis and Treatment [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism in American Males: Symptoms, Monitoring, and Management Strategies [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism: Impact on Mood and Treatment in American Men [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Secondary Hypogonadism: Causes, Symptoms, and Comprehensive Management Strategies [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Managing Secondary Hypogonadism: Diagnosis, Hormonal Therapy, and Lifestyle Strategies for American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Secondary Hypogonadism: Impact on Energy, Vitality, and Treatment Options for American Men [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Secondary Hypogonadism in American Males: Weight Management and Holistic Health Strategies [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Managing Secondary Hypogonadism: The Crucial Role of Diet and Nutrients [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Managing Secondary Hypogonadism: Diagnosis, Treatment, and Enhancing Quality of Life [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Secondary Hypogonadism: Impacts on Men's Relationships and Management Strategies [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Secondary Hypogonadism in American Males: The Critical Impact of Sleep Deprivation [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Secondary Hypogonadism: A Holistic Approach for American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Secondary Hypogonadism's Impact on Mental Clarity in American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Community Support's Vital Role in Managing Secondary Hypogonadism in American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Secondary Hypogonadism's Impact on Emotional Resilience in American Men [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Managing Secondary Hypogonadism: A Holistic Approach for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Understanding and Managing Secondary Hypogonadism in American Males [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Secondary Hypogonadism in American Males: Diagnosis, Treatment, and Personalized Care [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Secondary Hypogonadism's Impact on Mental Health in American Males: Diagnosis and Treatment [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Understanding Secondary Hypogonadism: Causes, Symptoms, and Management for American Males [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Causes, and Management Strategies for American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Secondary Hypogonadism: Impacts on Muscle, Bone, and Cardiovascular Health in American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Secondary Hypogonadism's Impact on Self-Esteem in American Men: Causes and Management [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Understanding, Diagnosing, and Enhancing Vitality in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Understanding Causes, Symptoms, and Management in American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Importance of Regular Health Check-ups for American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Lifestyle Factors and Secondary Hypogonadism: Impacts and Prevention Strategies for American Males [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Secondary Hypogonadism: Emotional Impact and Comprehensive Management in American Men [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Secondary Hypogonadism in American Men: Symptoms, Impacts, and Management Strategies [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
- Secondary Hypogonadism: Impacts on Health and Importance of Early Detection in Men [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
Word Count: 548