Introduction
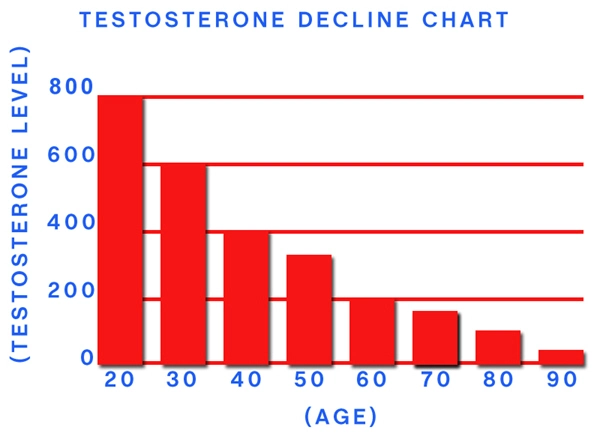
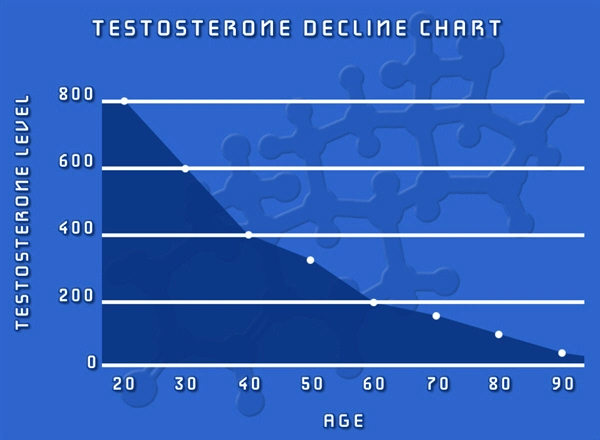
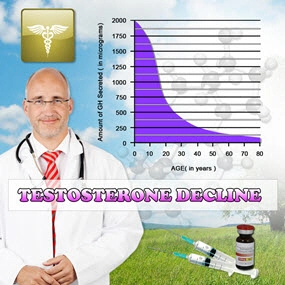
Late-onset hypogonadism (LOH), also known as age-related hypogonadism, is a clinical and biochemical syndrome characterized by a deficiency in serum testosterone levels in conjunction with associated symptoms. This condition has been increasingly recognized as a significant health concern among aging American males. Concurrently, diabetes mellitus, a metabolic disorder characterized by elevated blood glucose levels, has reached epidemic proportions in the United States. Recent research has begun to explore the potential connections between these two conditions, shedding light on their intertwined pathophysiology and clinical implications.
The Prevalence of Late-Onset Hypogonadism and Diabetes
In the United States, the prevalence of LOH among men over the age of 40 is estimated to be between 20% and 40%. Similarly, diabetes affects approximately 10.5% of the American population, with a higher incidence among males. The coexistence of these conditions in the same individual is not uncommon, and studies have shown that men with diabetes are at an increased risk of developing LOH.
The Pathophysiological Connection
The relationship between LOH and diabetes is multifaceted and involves several interconnected pathways. Insulin resistance, a hallmark of type 2 diabetes, has been shown to be associated with decreased testosterone levels. Conversely, low testosterone levels can contribute to the development of insulin resistance and impaired glucose metabolism. This bidirectional relationship suggests that LOH and diabetes may perpetuate each other, leading to a vicious cycle of metabolic dysfunction.
Furthermore, obesity, a common risk factor for both conditions, plays a significant role in their pathogenesis. Adipose tissue produces aromatase, an enzyme that converts testosterone to estradiol, leading to a decrease in bioavailable testosterone. Additionally, obesity is associated with increased inflammation and oxidative stress, which can further contribute to the development of both LOH and diabetes.
Clinical Implications and Management
The recognition of the link between LOH and diabetes has important clinical implications for the management of American males affected by these conditions. Routine screening for LOH in diabetic patients, particularly those with symptoms such as decreased libido, erectile dysfunction, and fatigue, may be warranted. Similarly, men diagnosed with LOH should be evaluated for the presence of diabetes or prediabetes.
Lifestyle modifications, including weight loss, regular exercise, and a healthy diet, are crucial in the management of both LOH and diabetes. These interventions can help improve insulin sensitivity, reduce inflammation, and increase testosterone levels. In some cases, testosterone replacement therapy (TRT) may be considered for men with confirmed LOH, as it has been shown to improve glycemic control and insulin sensitivity in diabetic patients. However, the use of TRT in diabetic men should be carefully monitored, as it may also increase the risk of certain cardiovascular events.
Future Directions and Research
The connection between LOH and diabetes in American males is an area of ongoing research and clinical interest. Future studies should focus on elucidating the underlying mechanisms of this relationship, identifying novel therapeutic targets, and developing personalized treatment approaches. Additionally, long-term studies are needed to assess the impact of TRT on cardiovascular outcomes in diabetic men with LOH.
Conclusion
The link between late-onset hypogonadism and diabetes in American males represents a significant public health concern. The intertwined pathophysiology of these conditions underscores the importance of a comprehensive approach to their management, including lifestyle modifications, regular screening, and, when appropriate, targeted therapies. By recognizing and addressing this connection, healthcare providers can improve the overall health and quality of life of affected individuals.
Contact Us Today For A Free Consultation

- Exploring Alternatives to TRT for Late-Onset Hypogonadism in American Males [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Nutrition's Role in Managing Late-Onset Hypogonadism in American Males [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Future of Late-Onset Hypogonadism Treatment: Innovations and Personalized Approaches [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Late-Onset Hypogonadism: Impact on Mood, Energy, and Quality of Life in American Men [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Genetic Insights into Late-Onset Hypogonadism in Aging American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Late-Onset Hypogonadism: Effects on Muscle Mass and Treatment Options in American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Late-Onset Hypogonadism: Prevalence, Economic Impact, and Management Challenges in American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Late-Onset Hypogonadism: Symptoms, Diagnosis, and Management in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Preventing Complications of Late-Onset Hypogonadism in American Men: Strategies and Insights [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Late-Onset Hypogonadism: Impact on Fertility and Health in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Exercise as a Key Strategy for Managing Late-Onset Hypogonadism in American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Late-Onset Hypogonadism: Early Detection and Management in American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hormone Replacement Therapy for Late-Onset Hypogonadism: Benefits, Risks, and Guidelines [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Understanding and Managing Late-Onset Hypogonadism in American Men Over 40 [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Managing Late-Onset Hypogonadism: Emotional Challenges and Support for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Stress Exacerbates Late-Onset Hypogonadism in American Males: Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Understanding Late-Onset Hypogonadism: Impacts and Management in Aging Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Late-Onset Hypogonadism: Understanding Symptoms, Impacts, and Management Strategies for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Late-Onset Hypogonadism: Impact on Sleep and Holistic Management Strategies for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Late-Onset Hypogonadism's Cognitive Impact in American Men: Awareness and Management Strategies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Late-Onset Hypogonadism: Understanding TRT Benefits and Risks in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Understanding Late-Onset Hypogonadism: Symptoms, Impact, and Management for American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Managing Late-Onset Hypogonadism: Symptoms, Diagnosis, and Treatment Options for American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Dietary Strategies to Manage Late-Onset Hypogonadism in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Understanding Late-Onset Hypogonadism: Prevalence, Symptoms, and Management in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Late-Onset Hypogonadism: Symptoms, Diagnosis, and Management in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Late-Onset Hypogonadism: Prevalence, Risks, and Management in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Diagnosing Late-Onset Hypogonadism: Symptoms, Testing, and Challenges in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Late-Onset Hypogonadism: Overcoming Stigma and Enhancing Men's Health in America [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Understanding Late-Onset Hypogonadism: Symptoms, Impact, and Management for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Early Intervention Benefits for Late-Onset Hypogonadism in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Late-Onset Hypogonadism: Symptoms, Diagnosis, and Treatment for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Late-Onset Hypogonadism in American Males: Importance of Monitoring and Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Managing Late-Onset Hypogonadism: A Multidisciplinary Approach for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Advocating for Better Late-Onset Hypogonadism Care: A Call to Action for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Late-Onset Hypogonadism: Understanding, Managing, and Maintaining Independence in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Advanced Technology Enhances LOH Diagnosis in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Managing Late-Onset Hypogonadism: Symptoms, Diagnosis, and Treatment for Aging Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Late-Onset Hypogonadism: Diagnosis, Treatments, and Lifestyle Management for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Understanding Late-Onset Hypogonadism: Symptoms, Diagnosis, and Treatment for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Late-Onset Hypogonadism: Impact on Intimate Relationships and Management Strategies [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Late-Onset Hypogonadism: Symptoms, Diagnosis, and Management Strategies for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Cultural Perceptions and Management of Late-Onset Hypogonadism in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Understanding Late-Onset Hypogonadism: Myths, Facts, and Management for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Legal Aspects of Late-Onset Hypogonadism: Diagnosis, Treatment, and Rights in the U.S. [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Holistic Treatment of Late-Onset Hypogonadism in American Males: A Comprehensive Approach [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Late-Onset Hypogonadism: The Crucial Role of Mental Health Professionals [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Community Support Enhances Management of Late-Onset Hypogonadism in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Family Support Crucial for American Males with Late-Onset Hypogonadism [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Late-Onset Hypogonadism: Impacts and Strategies for Career Management in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Late-Onset Hypogonadism: Financial Implications and Management Strategies for American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Late-Onset Hypogonadism: Impact on Self-Esteem and Treatment Options for American Men [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Peer Support Enhances Life Quality for American Males with Late-Onset Hypogonadism [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Managing Late-Onset Hypogonadism: Lifestyle Strategies for American Men's Health [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Navigating Insurance Coverage for Late-Onset Hypogonadism: Diagnosis and Treatment Options [Last Updated On: April 3rd, 2025] [Originally Added On: April 3rd, 2025]
- Understanding Late-Onset Hypogonadism: Symptoms, Treatment, and Lifestyle Management for American Males [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Research Advances in Late-Onset Hypogonadism: Diagnosis, Treatment, and Lifestyle Impact [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Late-Onset Hypogonadism: Symptoms, Social Impact, and Management in American Men [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Late-Onset Hypogonadism: Symptoms, Diagnosis, and Management in American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Late-Onset Hypogonadism: Strategies for Mental Health in American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Late-Onset Hypogonadism: Stress, Nutrition, and Holistic Approaches for American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Late-Onset Hypogonadism in American Men: Advocacy and Personalized Care [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Nutritionists' Role in Managing Late-Onset Hypogonadism in American Males [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Exercise Strategies to Combat Late-Onset Hypogonadism in American Men [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Late-Onset Hypogonadism: Prevalence, Impact, and Management in American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Managing Late-Onset Hypogonadism: Symptoms, Diagnosis, and Treatment for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Late-Onset Hypogonadism: Understanding and Managing Emotional Impacts in Men Over 40 [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Endocrinologists' Vital Role in Managing Late-Onset Hypogonadism in Aging American Males [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Late-Onset Hypogonadism in American Men: Diagnosis, Treatment, and Management Strategies [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Managing Late-Onset Hypogonadism: Lifestyle and Medical Interventions for American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Late-Onset Hypogonadism in American Males: Symptoms, Diagnosis, and Comprehensive Care Strategies [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Holistic Management Strategies for Late-Onset Hypogonadism in American Men [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Managing Late-Onset Hypogonadism: Impact and Strategies for American Men's Sexual Health [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Late-Onset Hypogonadism: Impact, Research, and Future Directions in American Men's Health [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Managing Late-Onset Hypogonadism: Community Resources and Support for American Men [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Late-Onset Hypogonadism: Impact on American Men's Professional Lives and Management Strategies [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Therapists' Vital Role in Managing Late-Onset Hypogonadism in American Males [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
Word Count: 555