Video Link: https://vimeo.com/298622460
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/298623462
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
What is Hypogonadism?
Hypogonadism is a class of conditions which lead the testes to perform inadequately, either leading to the partial production or complete non-production of sperm, Testosterone, or both. There are two subdivisions of Hypogonadism—Primary and Secondary Hypogonadism. Primary Hypogonadism is caused by any medical issue which directly involves the testes and their inability to produce Sperm or Testosterone, even when adequately stimulated by precursor hormones. Secondary Hypogonadism, on the other hand, is the result of any condition which suppresses the production of precursor hormones, preventing the testes from getting the proper signal to produce sperm and/or Testosterone.
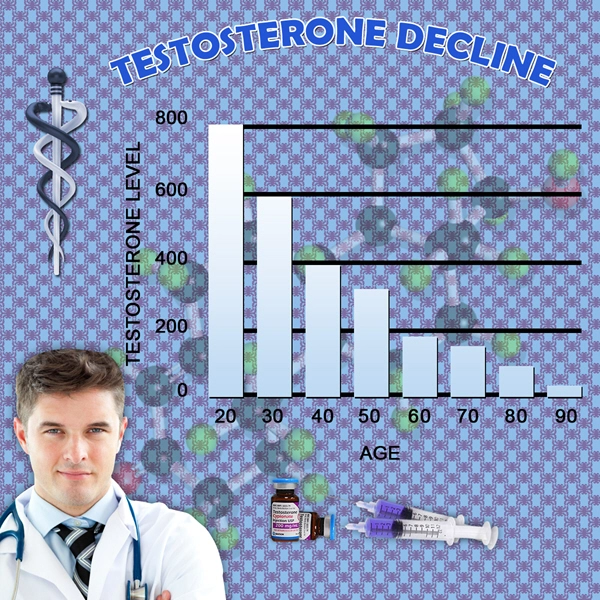
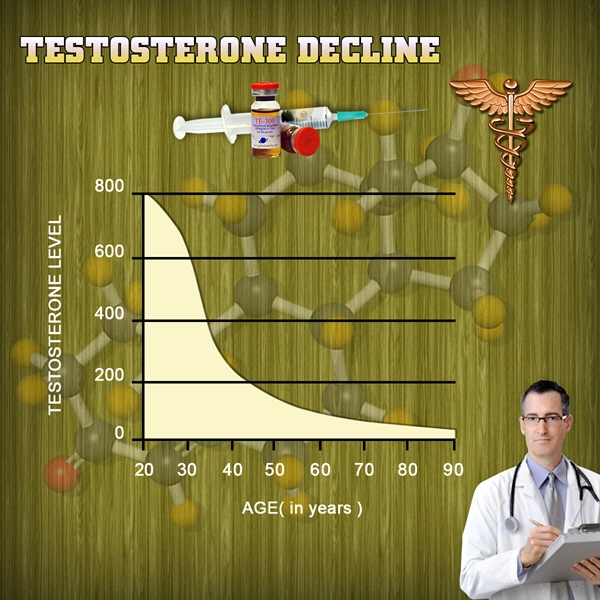
Among the most common forms of Hypogonadism is Age-Associated Testosterone Deficiency, a chronic condition which occurs naturally as men grow older, leading to a decline in the production of Testosterone. This condition is also referred to as Andropause. This form of Testosterone Deficiency cannot ultimately be prevented, but it can be put off for many years as a result of a healthy diet and exercise regimen and can occur earlier than average in men with poor lifestyles.
How is Hypogonadism Diagnosed and Treated?
Hypogonadism is diagnosed through two factors: the presence of symptoms of Testosterone Deficiency warrants concern, and blood testing confirms that the symptoms are the result of Low-T. Specific blood tests can differentiate between Primary and Secondary Hypogonadism, and other treatments may be necessary depending upon the ultimate source of the deficiency.
Testosterone Therapy should only be prescribed to patients that have been validly shown to need Low-T Treatment, and should not be prescribed without sufficient preliminary testing. Testosterone Treatments for Men have been shown to be both very useful and very safe for patients that have a valid need for the treatment resulting from hypogonadism, but for men with no established clinical need, the procedure can lead to unwanted risks and side-effects.
Free vs. Bound Testosterone
Testosterone that circulates through the bloodstream is either Free Testosterone or is linked to Albumin or Sex Hormone-Binding Globulin. The hormone is strongly attracted to SHBG and lightly drawn to Albumin. Most Testosterone is locked into SHBG, and only Free Testosterone can be actively used by the body. Only between one and three percent of Testosterone in the bloodstream is Free Testosterone.
What Stimulates Testosterone Production?
The secretion of Testosterone is facilitated through the interaction of Luteinizing Hormone with the testes. Luteinizing Hormone is released by the pituitary and activates at the testes. One form of Primary Hypogonadism is the result of the failure of the cells responsible for the production of Testosterone, known as Leydig Cells. This leads there to be abnormally high levels of LH in the bloodstream. If Luteinizing Hormone Levels are low or normal in combination with Testosterone Deficiency, this means that the deficiency is the result of upstream issues, and is often the result of medications, illness, and very commonly, the simple process of aging, itself.
When Should Testosterone Samples be Drawn?
Testosterone Levels are dependent upon the time of day. Every day, Testosterone Concentrations in the bloodstream rise and fall. These levels are at their highest in the morning and drop to their lowest a few hours after noon. There is evidence that the older that we get, the more that Testosterone Levels stabilize throughout the day, though these fluctuations remain present. When measuring Testosterone Levels for Low-T diagnosis, it is critical to test in the morning, preferably between the hours of eight and ten. Aging is also associated with an increase in SHBC-Linked Testosterone, resulting in a further decline in active, Free Testosterone concentrations.
What is Normal When it Comes to Testosterone Levels?
There is some debate regarding what is considered Normal Testosterone Levels. Different tests provide different expected scores, for example, and different age groups have different average Testosterone Levels. The generally accepted normal range for Testosterone is that which would be present in men between the ages of twenty and forty. The specific type of Testosterone measured is Serum Testosterone, that which is circulating through the bloodstream. Serum Testosterone Levels of below 350 nanograms per deciliter are considered deficient by most medical professionals, but many men will experience signs at levels at or slightly above this level.
Diagnosing Testosterone Deficiency
The first step in diagnosing Low-T is a medical history provided by the patient, along with a discussion of symptoms experienced. Next, the patient will undergo a physical, in which a variety of factors will be assessed, including breast size, body composition, the size of the testicles, and the distribution of body hair. The physician will also verbally screen the patient about any traumatic injuries involving the testes or the lower core of the body.
Beyond this point, a blood sample is taken from the patient. Many physicians will recommend taking blood samples on two different mornings. By analyzing Testosterone Levels, and the levels of Luteinizing Hormone and other factors, the prescribing doctor will be able to further narrow the potential causes of the deficiency, including genetic causes in younger patients.
There are also many health and lifestyle issues which can suppress the production of Testosterone. There are many medications, for example, and other health conditions such as diabetes, sleep apnea, obesity, sedentary activity-level, and poor nutrition that can also suppress Testosterone Levels, and levels can be restored to a healthier level by changing habits and lifestyle.
Who Should Consider Testosterone Therapy?
Any patient that has experienced health symptoms which are related to Testosterone Deficiency should talk to a medical professional about treatment. In particular, males forty years or older with Testosterone Levels lower than eight nanomoles per liter, or less than 15 nanomoles per liter in combination with elevated Luteinizing Hormone Levels (1.5x or more) should consider treatment. Many patients with Testosterone Production in this range can receive healthcare subsidies for their deficiency.
What is the Goal of Testosterone Therapy?
The ultimate goal of Low-T Treatment is merely to get Testosterone Levels back to that which would be considered normal for a healthy male patient between the  ages of 20 and 40. Too much Testosterone can lead to health issues, just as too little Testosterone, and, in the end, a balance must be struck to optimize the health of the patient.
ages of 20 and 40. Too much Testosterone can lead to health issues, just as too little Testosterone, and, in the end, a balance must be struck to optimize the health of the patient.
There is still some work to be done to define precisely how much Testosterone is needed to provide the exact level of benefit necessary to overcome the effects of Low-T, but we are close enough to that ideal where it is possible to effectively and safely treat the effects of Testosterone Deficiency through Restorative Testosterone Therapy. One particular study discovered that a daily dose of five grams or more of Testosterone Cream was needed to get Testosterone into the normal range effectively. Other forms of Low-T Treatment such as Testosterone Injections, Implants, and Patches can be just as effective.
Before starting a Testosterone Therapy Regimen, it is essential to discuss the pros and cons of specific Testosterone Therapy Treatment Options with the prescribing doctor before deciding concerning treatment.
Continued Monitoring of Testosterone Therapy Benefits and Effects
An essential aspect of Testosterone Treatment is that the patient must undergo periodic reevaluation to make sure that the treatment is working as intended. Some doctors bring their patients back for reassessment after two months, but many wait until after six months of treatment. After this second evaluation, the patient only needs to see their prescribing Hormone Doctor once per year, unless issues arise that warrant an appointment.
Benefits of Testosterone Therapy
For patients with clinically diagnosed Low-T, many benefits can result from the use of Testosterone Therapy, most notably improved mood, relief from Erectile Dysfunction, Increased Sex Drive, improved muscle mass, increased energy, weight loss, and increased bone mineral density. Testosterone Therapy may also confer benefits concerning cardiovascular and cognitive health, but more research is needed in these areas.
For older patients interested in Testosterone Therapy for Andropause, Testosterone Treatments are usually offered after the patient has been appropriately evaluated, and other causes of Low-T have been ruled out.
Side-Effects and Safety Advisories for Testosterone Treatment
Individual patients should not use Testosterone Therapy. Testosterone is not associated with an increased risk of Prostate Cancer, but patients with Prostate Cancer should not use Testosterone. Men with sleep Apnea should also not use Testosterone, nor should those with abnormally high Hematocrit Levels or breast cancer. These conditions may all be worsened by the use of Low-T therapy.
Testosterone, nor should those with abnormally high Hematocrit Levels or breast cancer. These conditions may all be worsened by the use of Low-T therapy.
Testosterone Treatments lead to an increase in PSA Levels, but this increase is not associated with any adverse health risks. Because high PSA Levels are a side-effect of Prostate Cancer, patients should have PSA checked before starting Testosterone Treatment.
Low-T Treatments have been hypothesized to be associated with an increased risk of cardiovascular events, but further analysis has shown that Testosterone can provide certain benefits to the cardiovascular system and that most issues are the result of elevated Estrogen Levels and RBC Counts, both of which can be effectively treated in order to enhance the safety of treatment.
Who Should Use Testosterone?
Testosterone should be prescribed to patients that have been adequately evaluated to suffer from abnormally Low Testosterone Levels, while also suffering from symptoms related to Low-T. Patients should never be prescribed Testosterone without diagnostic analysis. With the help of Testosterone Replacement, it is possible for male patients to experience improved health and wellness by restoring Testosterone Concentrations that are correlated with normal and healthy function.
There is growing evidence that many women can benefit from Testosterone Therapy, especially those suffering from significant issues with sexual health and ![]() libido. Women need much less Testosterone than men but can benefit from restoration to normal levels for their sex. In the future, as research becomes more robust concerning women, more Low-T Treatments will be made available to women.
libido. Women need much less Testosterone than men but can benefit from restoration to normal levels for their sex. In the future, as research becomes more robust concerning women, more Low-T Treatments will be made available to women.
If you are interested in Testosterone Therapy, many clinics specialize specifically in Hormone Restoration, including HGH Therapy, Testosterone, and Sermorelin Acetate. Consider talking to a professional about whether or not Testosterone can benefit your health and your life!
Contact Us Today For A Free Consultation

Word Count: 1677